The nervous system is truly the most incredible and adaptable biological system ever created. The nervous system is an intelligent design composed for bidirectional biological communication to ensure survival. I was fortunate enough to attend a course, Mobilization of the Neuroimmune System, this weekend to enhance my understanding of how to best recognize and approach a comprised nervous system.
Weekend Takeaways:
- The immune system heavily influences the nervous system
- Neurodynamic tests assess the physical capacity of the nervous system
- Active treatment is more than just moving it also includes breathing and learning.
- The type of biological container implicated matters for treatment approach
- "Rehab exercises" are not as much about strength as they are about homuncular clarity
In this post I want to explore the first take away to help illustrate briefly how the nervous system and immune system are related.
The Immune System Heavily Influences The Nervous System:
We got the weekend started by diving deep into the neurobiology of the nervous system and its relationship with the immune system. Traditionally these two systems have been viewed as separate entities, but that view is now stale, especially when pain enters the picture. It would now be appropriate to view the nervous system as a neuroimmune organ. Have you ever wondered why you get a whole body ache when you are sick? Or why your musculoskeletal pain worsens when sick? What about why your pain increases with a weather change? Each of these are due to an elevated neuroimmune system response based on past experiences. The immune system is a system that knows who you are and will intervene whenever you are not yourself. The immune system is very efficient as there are nearly ten times the amount of immune cells than there are neurons (nerve cells). This is a beautiful and efficient design for protection.
Unfortunately the initial response of the nervous system tends to be inflammation and a painful experience because they are most effective at altering behavior and reducing an imposed threat. But why does this occur with something as simple as a weather change or going on a walk? Well, the human brain never forgets. It has an amazing capacity to remember and store memories within the hippocampus. When memories are stored so are the emotions and the environmental context of the time. So when an event or environment is encountered the body will recall memories, the associated emotions, as well as the environmental context to predict an appropriate outcome. If there was a harmful experience in the past you may trigger an immune response. How? Interestingly enough, your emotions are derived from the amygdala and memories, the hippocampus, both of which are immune system mediators. This means that your past experiences can trigger immune responses and dictate how the nervous system responds.
How the nervous system responds is dependent upon the pathobiological mechanism, or how the brain processes the incoming information. There are two types of mechanisms: pain and tissue. The pain mechanism tends to be related to central processing and viewed as a top-down process. When this occurs there has become alterations in the central nervous system causing the brain to become too protective with its’ predications. There has become a belief there is more danger than there is in reality. Danger will evoke F.E.A.R (false evidence appearing real). Remember your emotions can trigger an immune response even if unnecessary. This in turn begins to make your nerves more sensitive and more irritable for the future.
Tip:
Often you can determine if there is a central processing issue by placing a hot pack on a painful region. If you think about it from a physiological perspective this should increase inflammation and make you feel WORSE! So if heat feels good be thankful because the tissue you think is damaged is likely not as bad as you think!
The tissue mechanism is related to peripheral processing, or a bottom-up process. This is the typical process during an acute injury and follows the predictable stages of healing. When a tissue is injured inflammation is sent locally to start the healing process. This inflammation triggers the neuron to fire a signal to the brain. If pain is the output, inflammation will be sustained to allow the tissue to heal. Remember inflammation is a protector. So when inflammation persists it will reduce the firing threshold of the neurons, making it easier for them to be triggered. This prevents you from further tissue damage, but makes you more likely to experience pain with normally non-painful activities. Interestingly though this is not just an acute scenario. Once you have healed completely, your body will leave some resident immune cells in the previously injured area just in case. This is why your body can remember your pain so well and allow a “relapse” to occur. Remember the brain never forgets and always predicts.
Tip:
We do not have pain receptors! We have nociceptors that send a signal to the brain where it is decided whether or not pain is the appropriate response. This is why tissue damage and pain rarely correlate!
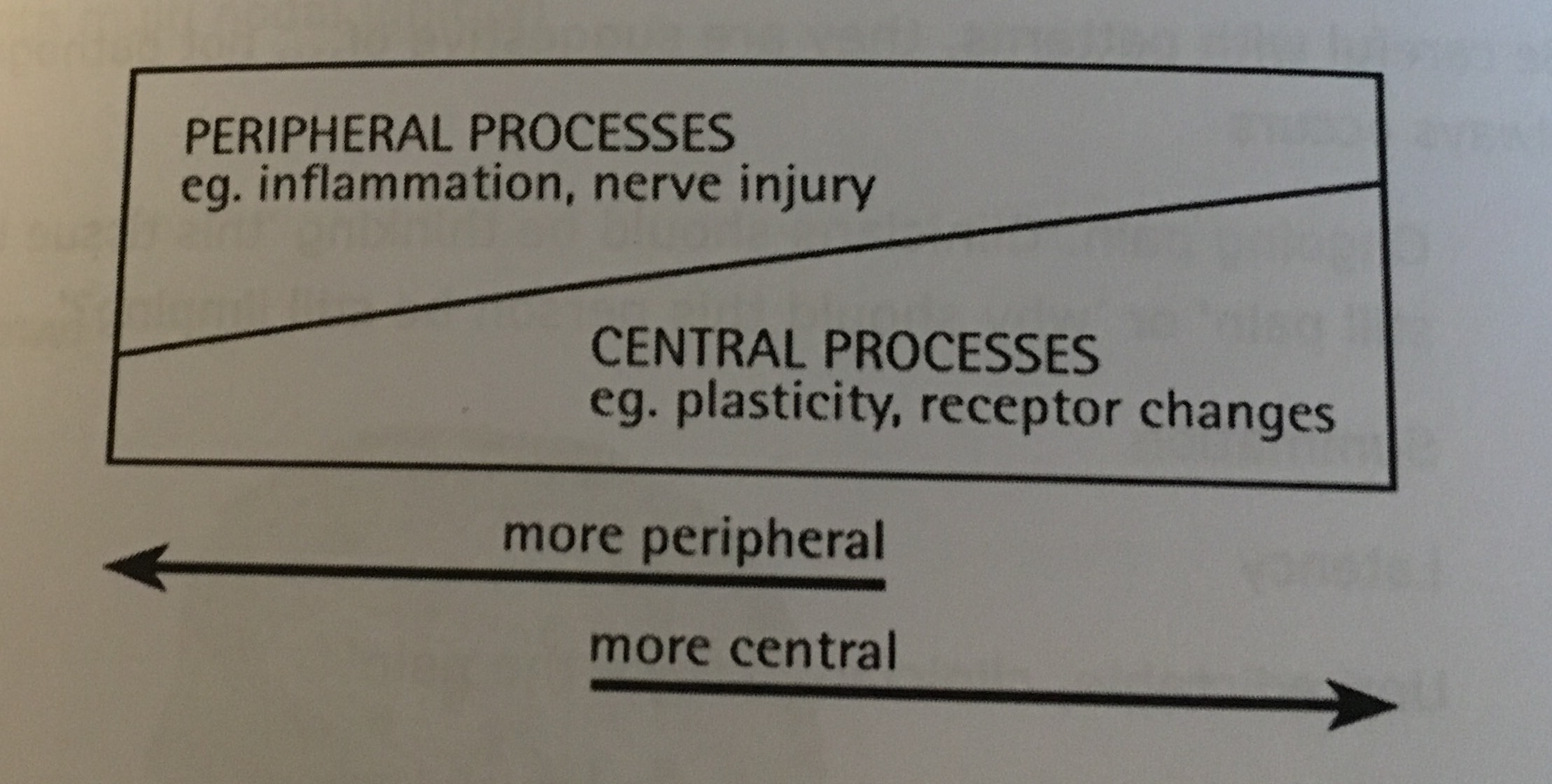
That being said, deciphering if it is a pain or tissue mechanism is not as simple as placing a hot pack and seeing what happens. Central and peripheral processes occur simultaneously, but which is the dominant player is the critical aspect. In part 2 of this series I will review how the use of Neurodynamic testing can help to illuminate the physical capacity of the nervous system and guide this clinical reasoning process.
Stay Well, Stay Strong
Keaton