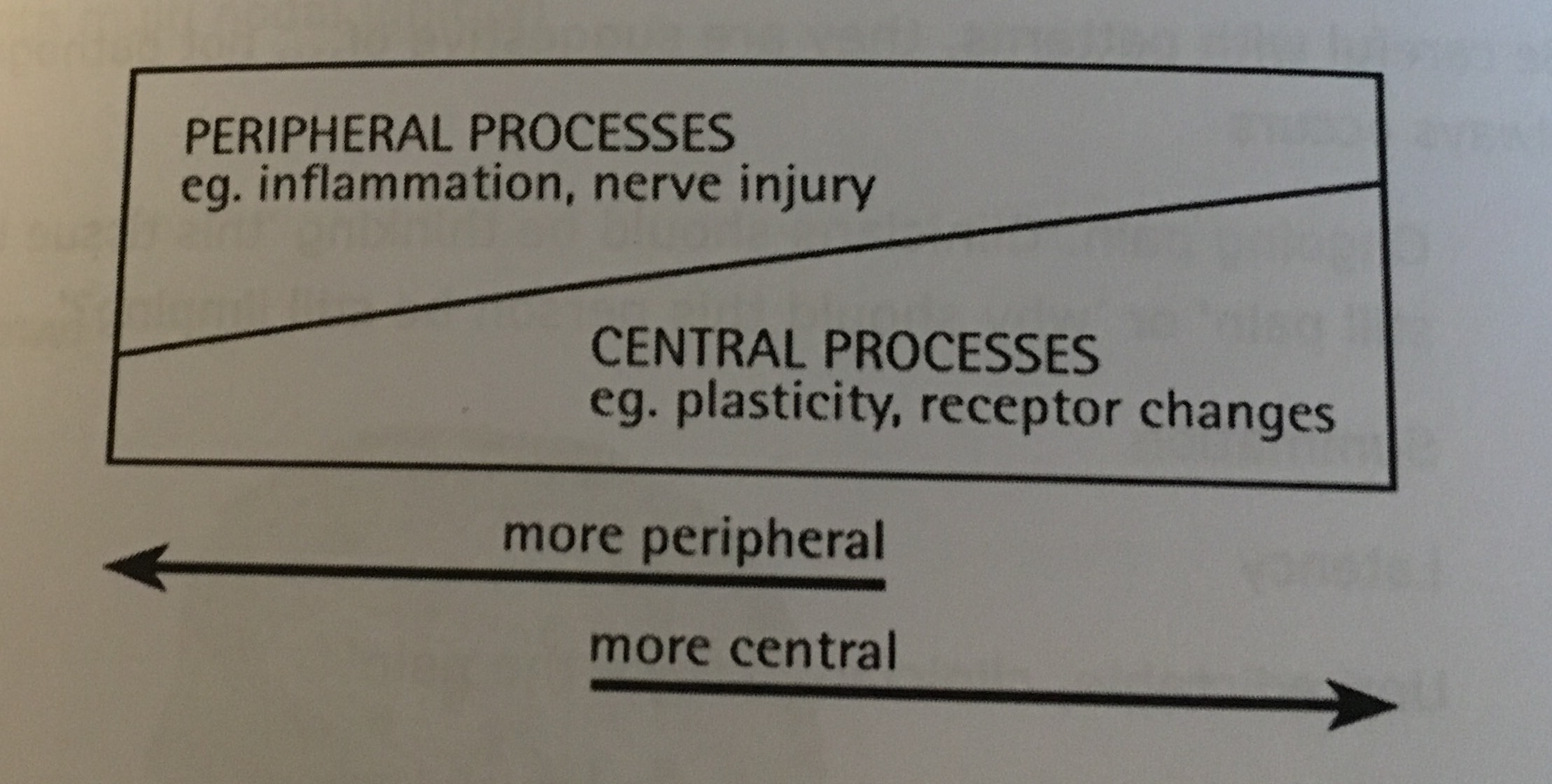
If there is one aspect of life that is often undervalued and under-appreciated it is sleep. Our ability to sleep is essential to allow a full resolution of pain and restoration of our movement. Our ability to sleep can be correlated to how our nervous system is being activated. We have 2 parts of our nervous system: sympathetic and parasympathetic. You see, when we are experiencing pain our nervous system becomes sensitized and preferential to the sympathetic nervous system. Now when this is the case you will see a rise in heart rate, blood pressure, respiration rate, and even anxiety. Sound familiar on those sleepless nights? You can loosely think of this activation of the sympathetic nervous system as if you drank a large cup of coffee or an energy drink right before bed. Most people would not choose to partake in such behavior because they would be up all night. This is the exact case for many of those who have had or are currently in a pain-cycle however it isn’t perceived as such. People who are experiencing sleep disturbances or find it difficult to become comfortable at night, please realize that the solution is on the other side of the nervous system: parasympathetic. There are numerous things we can control or change in the activities leading up to bed as well as with the sleep environment that will allow the parasympathetic nervous system to be tapped into.
According to the National Sleep Foundation, sleep hygiene is considered to be a variety of different practices and habits that are necessary to have good nighttime sleep quality and full daytime alertness. Sounds great, but what does this have to do with resolving pain and improving movement? Well, consider sleep as the foundation of your health and stress management. By purposefully improving sleep hygiene you are taking a step in regaining control of your life. Here’s how to do it:
1. Be regular and consistent with the time you get up.
That’s right when you get up opposed to when you go to sleep. The reason is that this will allow you to improve your sleep efficiency, the ratio of time in bed asleep opposed to in bed and awake. The first couple of days may be rough and you may feel fatigue during the day, but this should be reflected on the back end of the day because you will feel tired sooner and be able to determine your ideal bedtime. I guess you can say we are trying to reverse engineer your bed time.
2. Don’t oversleep.
Many people live by the idea that they can go on little to no sleep during the week and make up for it on the weekend. This is not the case. You cannot make up for your accumulated weekly sleep debt by sleeping in on the weekends or days off. What you are actually doing is setting yourself up for increased grogginess and fatigue throughout the day, which in turn could increase tension and amplify your aches and pains.
3. Create a positive psychological association with the bedroom.
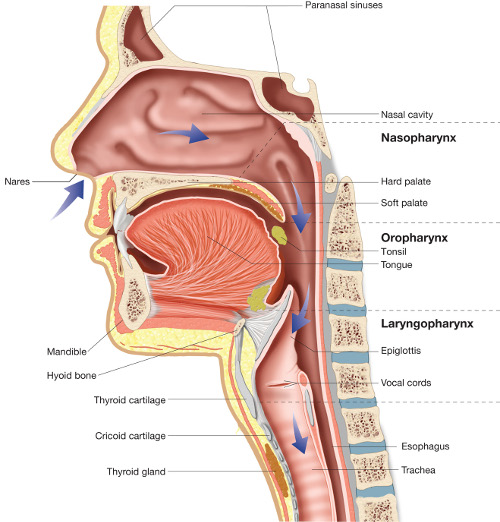
The purpose of a bedroom is two-fold: sleep and sex. If you currently reading, watching television, drinking a cup of tea, etc. before bed, work to try to move these activities to somewhere outside of the bedroom and prior to being ready for sleep. To perform these activities it requires an increase in alertness and attention, which are both associated with wakefulness and thus an increase in sympathetic activity.
4. Substance avoidance: alcohol, nicotine, or caffeine.
Alcohol is often regarded as the ideal nightcap beverage given that it is a depressant. This is true that it is a depressant, but what is often missed is that alcohol causes us to fall asleep faster than we normally would thus miss out on a portion of our REM (radpid eye movement) cycle. This is important because disruption of the REM cycle can alter the entire sleep-wake cycle and associated hormonal releases that help you both function and recover when injured.
With regards to nicotine and caffeine, they are both stimulants and will make it difficult to fall asleep. Now if your thinking I drink a cup of coffee before bed every night and don’t have any changes in my ability to sleep. I am here to tell you that this is likely due to you already being sympathetically driven and in need of a shift into more parasympathetic activity. Take the caffeine away and see if you notice a difference.
5. Can’t sleep, GET UP.
If you lay in bed unable to sleep for more than 20-30 minutes get up and perform some form of relaxation: meditation, breathing exercises, etc. Once you feel tired again return to your bedroom and go to sleep. The goal here is to keep the positive association with your sleeping environment.
6. Get rid of all your thoughts and worries.
A lot of people ponder their to do list for the next day or revisit a stressful part of work day that happened this only achieves a rise in heart rate and blood pressure. Take the 3-5 minutes before going to bed to let it all out in a journal so you can clear your mind before you sleep.
7. Create a sleeping environment.
Try to implement 1 or more of these sleep environment changes to optimizes your quality of sleep once you fall asleep.
















![Wieght-Loss1[1].jpg](https://images.squarespace-cdn.com/content/v1/542eadace4b0d41ade87d5be/1445528217453-H1YB8DCTJ1RS9G3EG8YX/Wieght-Loss1%5B1%5D.jpg)



