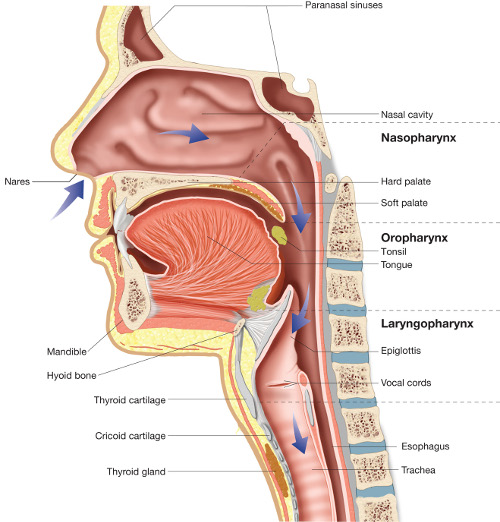
In Part 1 we discussed the airway and how it relates to the stress response at a general level. In part 2 we will discuss the airway at the level of the head and neck and how that affects stress and posture. The primary factors we will look at are Jaw position/bite, tongue position, and the nasal cavities.
The human body is very sensitive to the size of the airway.(1) The size of the airway dictates the brain’s perception of the environment as being safe or threatening. A small airway can result in a sensitive stress response as the oxygen demand will more quickly exceed the supply. Factors such as whether or not a child was breastfed and for how long, when a child was started on hard foods, and if a child uses a pacifier can all be related to the development size of one’s airway.(2,3,4) First, let’s talk about jaw position.
Jaw Position:
Research has been found that it only takes a two mm shift in jaw position to cause or alleviate sleep apnea. This is important because sleep apnea, which can lead to a state of low oxygen in the body, is commonly found in individuals with pain complaints.(5,6,7,8) A state of low oxygen is a massive stressor to the body.
Tongue Position
If a small shift in jaw position is enough to affect sleep and the airway, tongue size and position is important as well.(9) Tongues that are restricted because of tongue ties, tend to fall back in the airway easily especially during sleep.(10) Restricted tongues also affect development of the airway too. Larger tongues are more likely to fall back and block the airway during sleep.(11,12) The reason a tongue is large is often linked to how it is being used. Tongues can become large when allowed to relax and muscle tone is reduced. However, a tongue that is applying light pressure to the hard palate behind the incisors will actually take up less space and open up the airway.(12) The caveat is that the tongue cannot do this alone. It requires nose breathing.
Nasal Cavity
The nasal cavity is extremely important in regards to the airway. For instance nose breathing in and of itself helps to reduce blood pressure and decrease muscle activity that leads to shoulder and neck tightness.(13,14) A deviated nasal septum or a hole in the nasal septum is also a potential factor in air way obstruction.
There are many factors related to airway obstruction and how the airway is related to pain complaints. In this article we addressed three evidence based factors related to the airway and musculoskeletal pain. Though it is not always a requirement to have “ideal” tongue posture, jaw position, or nasal cavity, it can be important to consider each of these as possible factors related to pain complaints especially when one has had no results or recurrent episodes of pain complaints.
As always, take care and breathe easy!
Dave
References
Izuka EN, Feres MF, Pignatari SS. Immediate impact of rapid maxillary expansion on upper airway dimensions and on the quality of life of mouth breathers. Dental Press J Orthod. 2015;20(3):43-9.
Brew BK, Marks GB, Almqvist C, Cistulli PA, Webb K, Marshall NS. Breastfeeding and snoring: a birth cohort study. PLoS ONE. 2014;9(1):e84956.
Page DC. Breastfeeding is early functional jaw orthopedics (an introduction). Funct Orthod. 2001;18(3):24-7.
Howard CR, Howard FM, Lanphear B, et al. Randomized clinical trial of pacifier use and bottle-feeding or cupfeeding and their effect on breastfeeding. Pediatrics. 2003;111(3):511-8.
Nijs J, Loggia ML, Polli A, et al. Sleep disturbances and severe stress as glial activators: key targets for treating central sensitization in chronic pain patients?. Expert Opin Ther Targets. 2017;21(8):817-826.
Köseoğlu Hİ, İnanır A, Kanbay A, et al. Is There a Link Between Obstructive Sleep Apnea Syndrome and Fibromyalgia Syndrome?. Turk Thorac J. 2017;18(2):40-46.
Silva A, Mello MT, Serrão PR, et al. Influence of Obstructive Sleep Apnea in the Functional Aspects of Patients With Osteoarthritis. J Clin Sleep Med. 2018;14(2):265-270.
Martinot JB, Borel JC, Cuthbert V, et al. Mandibular position and movements: Suitability for diagnosis of sleep apnoea. Respirology. 2017;22(3):567-574.
Yoon AJ, Zaghi S, Ha S, Law CS, Guilleminault C, Liu SY. Ankyloglossia as a risk factor for maxillary hypoplasia and soft palate elongation: A functional - morphological study. Orthod Craniofac Res. 2017;20(4):237-244.
Harvey R, O'brien L, Aronovich S, et al. Friedman tongue position and cone beam computed tomography in patients with obstructive sleep apnea. Laryngoscope Investig Otolaryngol. 2017;2(5):320-324.
Barrera JE, Pau CY, Forest VI, Holbrook AB, Popelka GR. Anatomic measures of upper airway structures in obstructive sleep apnea. World J Otorhinolaryngol Head Neck Surg. 2017;3(2):85-91.
Hwang DM, Lee JY, Choi YJ, Hwang CJ. Evaluations of the tongue and hyoid bone positions and pharyngeal airway dimensions after maxillary protraction treatment. Cranio. 2018;:1-9.
Gelardi M, Abbattista G, Quaranta VN, et al. Standardization procedure for the nasal nitric oxide measurement method using Niox MINO® and the tidal-breathing technique with velum-closure. J Biol Regul Homeost Agents. 2016;30(3):853-858.
Ip MS, Lam B, Chan LY, et al. Circulating nitric oxide is suppressed in obstructive sleep apnea and is reversed by nasal continuous positive airway pressure. Am J Respir Crit Care Med. 2000;162(6):2166-71.